In an era of increasing emphasis on sustainable development, countries worldwide face a complex and critical challenge in the design and construction of operating rooms: how to uphold the fundamental principle of infection control while simultaneously addressing economic efficiency and environmental responsibility. Although infection control, cost-effectiveness, and environmental sustainability may appear to be competing priorities, they must be pursued in a coordinated and integrated manner. Due to variations in healthcare systems, economic conditions, and environmental policies, different nations have adopted distinct approaches and strategic emphases.

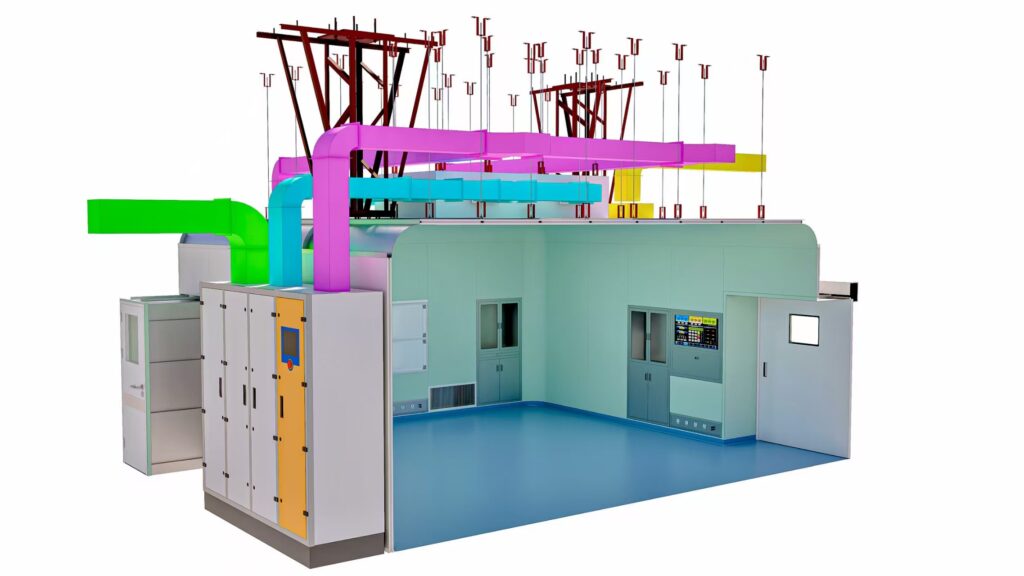
In China, operating room construction adheres strictly to the mandatory national standard “Architectural Technical Code for Hospital Clean Operating Department” (GB 50333-2013), with a focus on precision infection control, intelligent operation and maintenance, and life-cycle cost optimization. In terms of infection prevention, high-efficiency air purification technologies—such as ULPA and HEPA filters—are employed alongside rigorous functional zoning to establish robust contamination barriers. For cost management, initial investment in high-standard infrastructure is prioritized to minimize long-term operational and maintenance expenses. Energy-saving strategies include optimizing HVAC system performance during non-peak hours and upgrading lighting systems. Environmentally, efforts center on promoting modular cleanroom technologies to enhance flexibility and resource efficiency.
The United States emphasizes source-based infection prevention, particularly through foundational practices such as hand hygiene and aseptic techniques. This approach is complemented by integrating procedural management with engineering controls, rather than relying solely on ultra-clean ventilation. Engineering solutions are selected based on cost-benefit analysis—for example, using energy-efficient air distribution systems while avoiding excessive investments in unidirectional airflow technology where not clinically justified. Waste reduction is achieved through systematic waste segregation and the increased use of reusable surgical instruments. Furthermore, the widely adopted “Central Core” layout places sterile supply areas at the center, surrounded by multiple operating rooms. This configuration streamlines material logistics, reduces the distances for retrieving items, limits unnecessary personnel movement, and thereby enhances both operational efficiency and infection control.
The United Kingdom adopts a balanced strategy that combines engineering interventions with preventive protocols, advocating for ultra-clean ventilation in high-risk procedures. Laminar airflow systems and UVC disinfection are commonly deployed in specific surgical contexts, guided by stringent regulatory frameworks such as Health Technical Memoranda 00-00: Policies and Principles of Healthcare Engineering. Cost management follows a life-cycle perspective, ensuring consistency across planning, construction, commissioning, and operational phases to avoid short-term savings that lead to long-term inefficiencies. Environmental initiatives include the implementation of advanced energy management systems and the selection of low-global-warming-potential anesthetic gases, embedding sustainability throughout clinical workflows.

Despite national differences in implementation, a convergent trend is evident in modern operating room design: a shift from the historical paradigm of “maximum cleanliness at any cost” toward a risk-informed, evidence-based, and systematically managed approach. This evolution can be distilled into three core principles:
First, maintain infection control as the non-negotiable priority while optimizing resource allocation. All cost-reduction and sustainability initiatives must preserve patient safety and clinical efficacy. Resources should be strategically directed toward interventions proven to reduce surgical site infections—such as hand hygiene compliance, thorough environmental decontamination, and strict separation of clean and contaminated pathways.
Second, apply life-cycle cost analysis and implement risk-stratified facility design. Given that contact transmission remains the primary route of surgical infections, disproportionate investment in air filtration systems is unjustified. A scientifically tiered classification of operating rooms—aligned with procedural risk levels—enables efficient resource deployment. High-level operating rooms should be designed for versatility, capable of supporting lower-complexity procedures, thereby improving utilization rates. Long-term value should guide procurement decisions, favoring technologies such as LED lighting and smart HVAC systems that entail higher upfront costs but deliver substantial energy savings and reduced maintenance over time.
Third, embed sustainability as a strategic objective to drive efficiency and reduce environmental impact. Environmental stewardship aligns closely with operational excellence. Cross-departmental collaboration and organizational culture change are essential to institutionalize energy conservation and waste minimization—such as standardized waste sorting and powering down non-essential equipment during idle periods. Technological integration, including IoT-enabled sensors for real-time monitoring of environmental conditions, allows for demand-responsive operation, such as reducing ventilation rates when rooms are unoccupied. Optimizing surgical scheduling further enhances space utilization. Additionally, automated terminal disinfection systems, modular construction units, and antimicrobial, easy-to-clean surface materials collectively reduce bioburden and resource consumption. As minimally invasive and digital surgery advance, seamless integration between environmental control systems (e.g., HVAC) and hospital information platforms becomes imperative for precise, data-driven environmental management.

The ideal model of modern operating room construction achieves equilibrium among infection prevention, economic viability, and environmental sustainability. By leveraging scientific classification, appropriate energy-efficient technologies, intelligent operational strategies, and rigorous management protocols, it is possible to develop high-performance operating room environments that are both clinically safe and resource-responsible.
Looking ahead, global operating room development will transcend incremental technological upgrades, moving toward holistic, integrated systems. Intelligence, precision, and sustainability will converge as defining characteristics of next-generation facilities. Big data analytics and artificial intelligence will enable dynamic optimization of personnel, equipment, and energy use, forming the foundation of intelligent operation and maintenance systems. Embracing circular economy principles—through enhanced material recyclability and equipment upgradability—will reduce environmental footprints. Flexible, adaptable designs will future-proof facilities against evolving medical demands, minimizing the need for costly retrofits and redundant construction.
Notably, innovative models such as the barn operating room and ambulatory surgery centers have gained traction in developed nations and are being piloted globally. These models achieve significant improvements in efficiency by reengineering clinical workflows and optimizing spatial layouts. Through shared infrastructure, they reduce per-procedure infection control costs and energy consumption while maintaining high safety standards. Such innovations exemplify effective reconciliation of the three core challenges. More than technological advancements, they represent the emergence of a next-generation operating room ecosystem — one that integrates cutting-edge technology, human-centered design, lean operations, and sustainable development.




